OFF TO JAKARTA AGAIN! With fresh eyes...
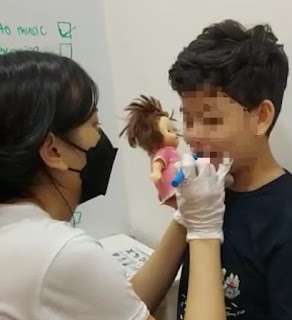
Finally! After 2 years 8 months, I made my first overseas consultation trip last week. It was to Jakarta, Indonesia.
The four kids whom I have been working with are no longer kids! Within the last two years, they have grown from tweens to teens (and one of them entered adulthood)! They are now all taller than me, have facial hairs and deeeeeep manly voices.
It was a joy to see them again. And I was super delighted to see them with fresh eyes. My fresh eyes are eyes of Orofacial Myofunctional Therapy (OMT).
Summer's specialises in Orofacial Myofunctional Therapy!
Two of us have each undergone 30 hours of specialised training in OMT.
Being a specialist in OMT, all of the sudden, I noticed many more recessed jaws, over used chin muscles, flanged lips, posterior tongue ties, low tongue placements, dried cracked lips, dark eye circles and many more. The 'perfect' tongue lateralisations and elevations were no longer perfect. The 'perfect' blowing were no longer perfect!
All the four kids have low resting tongues, overbites, and dried cracked lips. They have shallow breathing and difficulty with regulation. These are signs and symptoms of Orofacial Myofunctional Disorders (OMDs).
According to the Amercian Speech and Hearing Association (ASHA),
- OMDs are patterns involving oral and orofacial musculature that interfere with normal growth, development, or function of orofacial structures, or call attention to themselves (Mason, n.d.A).
- OMDs can be found in children, adolescents, and adults.
- OMDs can co-occur with a variety of speech and swallowing disorders.
- OMD may reflect the interplay of learned behaviors, physical/structural variables, genetic and environmental factors (Maspero, Prevedello, Giannini, Galbiati, & Farronato, 2014).
ASHA also listed the signs and symptoms of orofacial myofunctional disorders:
- Open mouth, habitual lips-apart resting posture (in children, adolescents, and adults)
- Structural abnormalities
- Restricted lingual frenulum (also known as tongue ties)
- Dental abnormalities, such as excessive anterior overjet, anterior, bilateral, unilateral, or posterior open bite, and under bite
- Abnormal tongue rest posture, either forward, interdental, or lateral posterior (unilateral or bilateral), which does not allow for normal resting relationship between tongue, teeth, and jaws, otherwise known as the interocclusal space at rest, or the freeway space (Mason, 2011)
- Distorted productions of /s, z/ often with an interdental lisp. Abnormal lingual dental articulatory placement for /t, d, l, n, ʧ, ʤ, ʃ, ʓ/
- Drooling and poor oral control, specifically past the age of 2 years
- Nonnutritive sucking habits, including pacifier use after age of 12 months, as well as finger, thumb, or tongue sucking (Warren & Bishara, 2002; Warren, et al., 2005; Zardetto, Rodrigues & Stefani, 2002)
- Lack of a consistent linguapalatal seal during liquid, solid, and saliva swallows.
- Interdental lingual contact or linguadental contact with the anterior or lateral dentition during swallows.
One of the major things I observe in all the four Jakarta 'kids' is mouth breathing. Mouth breathing is NOT normal. Nose breathing is.
Mouth breathing leads to the following problems in children:
- slower than normal growth rate
- poor regulation
- increased crying episodes at night
- large tonsils
- dry, cracked lips
- problems concentrating in school
- daytime sleepiness
- hyperactivity
Are these not the common 'complaints' we get from parents as well? OMDs are very common in our children with special needs, and they have huge huge huge impact on their development.
My goal henceforth will be to have all these four Jakarta 'kids' breathe through their noses. Can't wait to be back there again. And of course, for the food too...
Do find out more about OMDs and OMT at ASHA's website https://www.asha.org/practice-portal/clinical-topics/orofacial-myofunctional-disorders. If you suspect that your child has signs and symptoms of OMDs, do seek help from a Speech Therapist who specialises in OMT, i.e. Orofacial Myofunctional Therapy. Not all Speech Therapists are trained or specialise in OMT, or even Oral Motor Therapy.
#orofacialmyofunctionaltherapy #orofacialmyofunctionaldisorders #nosebreathing #mouthbreathing #tongueties #tetheredoraltissues #specialneeds #drooling #speechdelay #speechdisorders




Comments
Post a Comment